current research and writing
selected works in process
Healthy and Sick Life
Attentive to experiences of bodily life in sickness and in health, and orienting the excellences, or habits, that might enable a realistic philosophy and practice of medicine, this book offers a study of physicians and patients who confront health in sickness and who (ought to) correspond creatively, while giving shape to the respective vocations of physicianship and patienthood. Put differently, as a hermeneutic and phenomenological examination, and as a study in the philosophy and practice of medicine, Healthy and Sick Life concentrates on the life of sickly bodies caught up into communities of caring strangers—who are their healthy and sickly bodies too—in order to understand corporeality, communality, and the art of medicine.
The Dual Risk of Doctoring: Ontological Harm and the Shock of Medicine (with Jordan Mason and Andy Michel)
This paper responds to Sven Schaepkins and Anna Cianciolo’s call for philosophy in medical education to uncover “secret affinities” capable of unsettling medicine’s self-assured moral categories. Drawing Walter Benjamin’s account of Dadaist shock into conversation with phenomenological narratives of illness and healing, we argue that harm in medicine is not an aberration to be ethically avoided but an ontological reality intrinsic to the vocation of doctoring. Like Dadaism’s conversion of the artwork into a “missile,” medical practices—whether anatomical dissection, diagnosis, or intervention—annihilate the contemplative distance that sustains the illusion of detached mastery. The resulting tactile shock disrupts the being of both patient and practitioner, initiating a process of existential unmaking and remaking. Through engagement with Jean-Luc Nancy, Havi Carel, Amy Silverstein, and others, we develop the notion of ontological harm as the lived disturbance through which one’s relation to body, world, and time is altered. Such harm is neither failure nor exception but the very ground upon which fidelity, courage, and suffering-with can emerge. We contend that medical education must cultivate pedagogies that acknowledge, rather than anesthetize, this formative disruption. To train physicians is therefore not to shield them from harm but to prepare them for the dual risk of doctoring: that they will harm and be harmed, and that through this mutual exposure they may be awakened to a more humane, responsive, and faithful practice of care. Medicine thus becomes less a project of securing control and more a vocation of consenting to be implicated—an art that labors with the dust, bearing witness to healing within the shock of finitude.
The Physician as Innovator? Professional Identity and Practice Amidst Technological Advances (with Jordan Mason and Kyle Karches)
The professional role of physicians is evolving, as it always has, in the context of technological innovations. Recent reports advocate for the adoption of and collaboration with automated systems in medicine. While these innovations promise enhanced diagnostic accuracy, this paper argues that the underlying discourse often misinterprets the physician's role as an innovator, equating innovation with the mere consumption of technology. Drawing on philosophical insights and existing literature, the paper challenges the prevailing consumptive notion of "innovation" and explores the implications of this technological imperative on the physician's professional identity. We contrast the passive adoption of new technology, behavior associated with the “automaton,” with the active, virtuous agency of the "architektōn" or craftsperson, and call for a re-evaluation of what it means to be an innovator in medicine. Ultimately, we seek to reclaim the physician's role as a master striving to perform the excellences of their craft and capable of integrating new technologies with wisdom and skill, rather than being subsumed by them.
Atonement in Professional Life: Conceptualizing Physician Restoration after Medical Error (with Carl Hildebrand)
Medical error is a reality within medical practice because human practitioners are inherently fallible. While the consequences for patients are often immediate and severe, the enduring moral and existential impact on physicians is less visible while often profound. This paper argues that existing frameworks oriented around forgiveness are not best suited for guiding physicians toward moral restoration after error. Drawing on Alasdair MacIntyre’s conception of practice and virtue, we propose atonement as a central moral practice within medicine. Unlike forgiveness, which relies upon the response of the injured party, atonement is understood as an active, agent-centered process by which physicians can acknowledge error, make amends, and restore their professional and moral identity. We critically assess the limitations of both institutional responses and rituals such as Mortality and Morbidity conferences and offer a revised account of atonement comprising repentance, apology, reparation, and ongoing commitment to care. We suggest that atonement should be cultivated through structured, communal practices that integrate ethical mentorship, institutional support, and opportunities for reflection. In so doing, we reconceive professional flourishing not as the absence of error, but as the capacity to confront and integrate error and therefore grow through failure. This approach reframes medical error as a pedagogical moment—central to the development of virtues such as humility, courage, and fidelity—and argues that atonement is integral to the moral formation and flourishing of physicians.
FORTHCOMING, Perspectives in Biology and Medicine (Accepted 25 November 2025).
Making Fun of Medicine: Learning from Holy Fools and Sacred Clowns to Resist Medicine's Principalities (with Benjamin Frush, Brewer Eberly, Jr and Thomas Sieberhagen)
The figure of the “medical clown” is a theologically and anthropologically charged vocation necessary for moral critique and healing in contemporary medicine. Drawing on the Oglala Sioux Heyoka and the circus clown, or holy fool, the authors distinguish between external critics—philosophers and theologians who unmask medicine’s principalities through folly—and internal actors—clinicians who subvert dehumanizing logics from within. Against corporate, efficiency-driven models that deform the healing vocation, both roles embody prophetic reversal, exposing absurdities and reorienting practice toward possibilities of redemption that could not otherwise be seen from within the logic of medicine’s current priorities and principalities. The holy fool destabilizes the status quo through provocative critique; the Heyoka, grounded in communal trust, rouses through loving contrariness. Together, they witness to medicine’s eschatological promises: healing as relational and resistant to commodification. By reclaiming the sacred work of “walking backwards,” these clowns and fools invite a re-formation of medical imagination, challenging and shaping practitioners who dwell with suffering to resist the seductions of a system that is forgetting its calling.
publications
from scholarly writing to magazine columns

advice and opinions
columns written for Broadview and Sojourners
Jan/Feb 2025


Advice for a reader who supports supervised injection sites in principle — but not in practice
March 2025
Advice for a reader who made a promise to aging parents but cannot keep.
April 2025
Advice for a reader who is conflicted about eating meat
April 2025




A reflection on the powers and principalities manipulating Columbia University with insights from Dorothee Sölle and William Stringfellow
June 2025
A reflection on the coercive influence of political power on the church and reminder of her role in the world.
July/August 2025
Advice for a reader confronted by the misinformation of friends and colleagues
Sept/Oct 2025


Advice for a reader confronting the tension of personal beliefs and corporate values
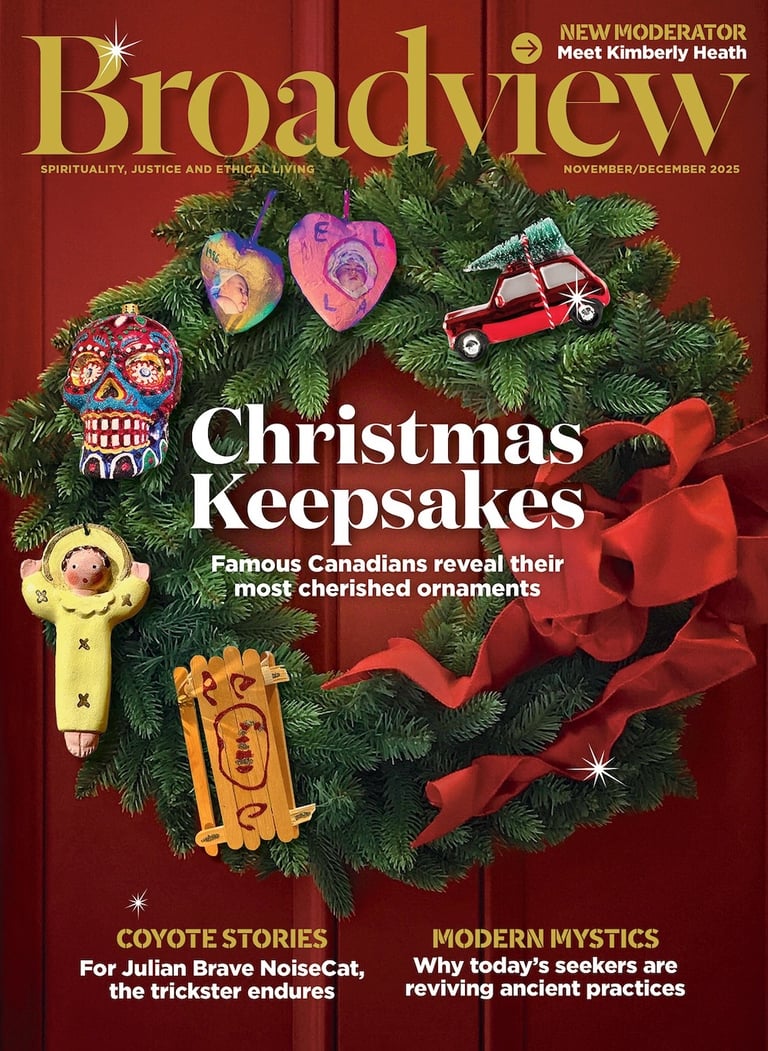
Nov/Dec 2025
Advice for a reader invited to a cross-border wedding but confronting the current political milieu
Jan/Feb 2026
Advise for a reader discerning how to distribute an estate given the social realities of poverty and inequity

publications
and scholarly efforts

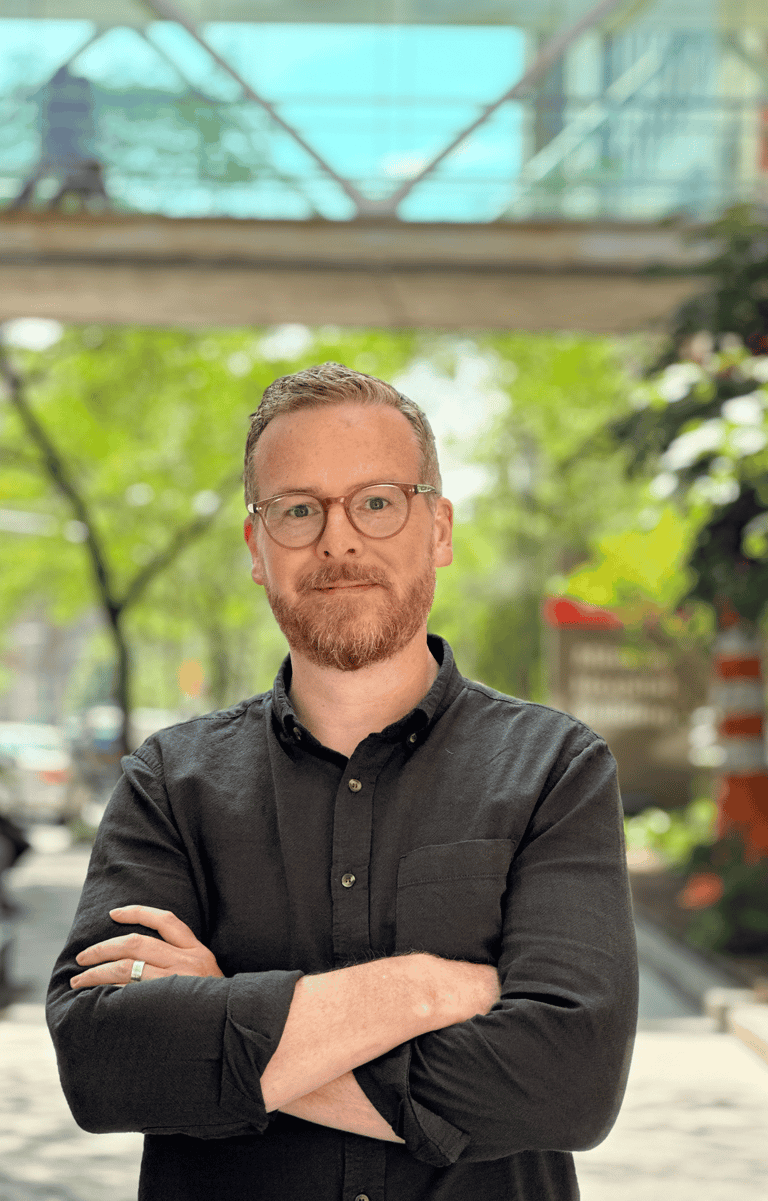
About
I am a Canadian (born and raised in Estevan, Saskatchewan) whose scholarly work tends to be found at the intersections of theology, philosophy, and medicine/health care. At present, I am the Associate Professor of Bioethics in the Department of Religion at Baylor University. I am concurrently a Research Fellow at Harris Manchester College, University of Oxford, a Research Associate at Vancouver School of Theology, and a Fellow with the James M Houston Centre for Humanity & the Common Good at Regent College.
Previously, I was the Assistant Professor of Medical Ethics and McDonald Scholar in the Center for Clinical Medical Ethics (directed by Dr Lydia Dugdale) at Columbia University Vagelos College of Physicians & Surgeons in NYC. At Columbia I was the intellectual curator and director of the Columbia Character Cooperatives (medical students) and the co-director with Dr Beatriz Desanti de Oliveira of the Character and Clinical Ethics Pathway (internal medicine residents), which were both novel educational programming in ethics education and professional/ moral formation. I also had the privilege of serve as the McDonald Postdoctoral Fellow in Christian Ethics and Public Life with the McDonald Centre for Theology, Ethics and Public Life at the University of Oxford, where I was also a senior member of Christ Church College. I was also appointed a humanities and healthcare fellow with a Wellcome Trust ISSF funded project, 'Advancing medical professionalism: integrating humanities teaching in the University of Oxford's medical school'. In addition to these recent roles, my academic background includes training in theology, bioethics and health policy, and applied physiology.
I owe a great deal to those scholars who've invested their time and energy into my academic formation, including Professors John C McDowell, Terry Lovat, Archie Spencer, Cad Dennehy, Carole Schneider (1950-2013), and Douglas Miller.